Breast Cancer Prevention (PDQ®): Prevention - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What Is Prevention?
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will reduce the burden of cancer and lower the number of deaths caused by cancer.
Cancer is not a single disease but a group of related diseases. Our genes, lifestyle, and the environment around us work together to increase or decrease our risk of getting cancer. Each person's cancer risk is made up of a combination of these factors.
To prevent new cancers from starting, scientists look at risk factors and protective factors. Anything that increases your chance of developing cancer is called a cancer risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk, but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied, including:
- Changing lifestyle or eating habits.
- Avoiding things known to cause cancer.
- Taking medicines to treat a precancerous condition or to keep cancer from starting.
- Having risk-reducing surgery.
General Information About Breast Cancer
Breast cancer is a disease in which malignant (cancer) cells form in the tissues of the breast.
The breast is made up of lobes and ducts. Each breast has 15 to 20 sections called lobes, which have many smaller sections called lobules. Lobules end in dozens of tiny bulbs that can make milk. The lobes, lobules, and bulbs are linked by thin tubes called ducts.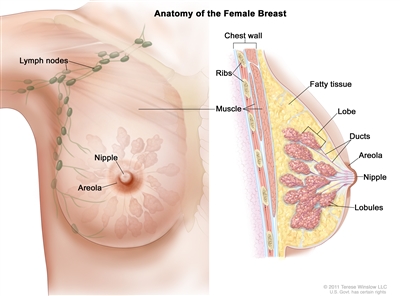
Anatomy of the female breast. The nipple and areola are shown on the outside of the breast. The lymph nodes, lobes, lobules, ducts, and other parts of the inside of the breast are also shown.
Each breast also has blood vessels and lymph vessels. The lymph vessels carry an almost colorless, watery fluid called lymph. Lymph vessels carry lymph between lymph nodes. Lymph nodes are small, bean-shaped structures that filter lymph and store white blood cells that help fight infection and disease. Groups of lymph nodes are found near the breast in the axilla (under the arm), above the collarbone, and in the chest.
Other PDQ summaries containing information related to breast cancer include:
- Breast Cancer Screening
- Breast Cancer Treatment
- Breast Cancer Treatment During Pregnancy
- Male Breast Cancer Treatment
- Genetics of Breast and Gynecologic Cancers (written for health professionals)
Breast cancer is the second leading cause of death from cancer in American women.
Women in the United States get breast cancer more than any other type of cancer except for skin cancer. Breast cancer is second to lung cancer as a cause of cancer death in American women. Breast cancer rates in women increased gradually for many years until the early 2000s and then decreased rapidly, coinciding with a drop in postmenopausal hormone therapy use. However, since 2005, there has been a small but steady increase in breast cancer rates in women. Deaths from breast cancer have declined by 42% as of 2021. However, breast cancer deaths in Black women remain about 40% higher than in White women. Breast cancer also occurs in men, but the number of new cases is small.
Breast Cancer Prevention
Avoiding risk factors and increasing protective factors may help prevent cancer.
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, having overweight, and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.
NCI's Breast Cancer Risk Assessment Tool uses a woman's risk factors to estimate her risk for breast cancer during the next five years and up to age 90. This online tool is meant to be used by a health care provider. For more information on breast cancer risk, call 1-800-4-CANCER.
The following are risk factors for breast cancer:
Older age
Besides being a woman, older age is the main risk factor for breast cancer. The chance of getting breast cancer increases as a woman gets older. A 30-year-old woman has about a 1 in 175 chance of being diagnosed with breast cancer in the next 10 years, while a 70-year-old woman has a 1 in 9 chance of getting the disease during the same time period.
Women aged 50 to 69 years who have screening mammograms have a lower chance of dying from breast cancer than women who do not have screening mammograms. Screening by mammography decreases breast cancer deaths by identifying cases for treatment at an earlier stage.
A personal history of breast cancer or benign (noncancer) breast disease
Women with any of the following have an increased risk of breast cancer:
- A personal history of invasive breast cancer, ductal carcinoma in situ (DCIS), or lobular carcinoma in situ (LCIS).
- A personal history of benign breast disease.
Inherited risk of breast cancer
Women with a family history of breast cancer in a first-degree relative (mother, sister, or daughter) have an increased risk of breast cancer.
Women who have inherited changes in the BRCA1 or BRCA2gene or in certain other genes have a higher risk of breast cancer. The risk of breast cancer caused by inherited gene changes depends on the type of gene mutation, family history of cancer, and other factors.
Dense breast tissue
Having breast tissue that is dense on a mammogram is a factor in breast cancer risk. The level of risk depends on how dense the breast tissue is. Women with very dense breasts have a higher risk of breast cancer than women with low breast density.
Increased breast density is often an inherited trait, but it may also occur in women who have not had children, have a first pregnancy late in life, take postmenopausal hormones, or drink alcohol. To learn more, visit Dense Breasts: Answers to Commonly Asked Questions.
Reproductive history resulting in greater exposure to estrogen
Estrogen is a hormone made by the body. It helps the body develop and maintain female sex characteristics. Being exposed to estrogen over a long time may increase the risk of breast cancer. Estrogen levels are highest during the years a woman is menstruating.
The following factors in a woman's reproductive history increase the length of time her breast tissue is exposed to estrogen and may increase the risk of breast cancer:
- Early menstruation: Beginning to have menstrual periods before age 12 increases the number of years the breast tissue is exposed to estrogen.
- Starting menopause at a later age: The more years a woman menstruates, the longer her breast tissue is exposed to estrogen.
- Older age at birth of first child or never having given birth: Pregnancy lowers a woman's lifetime number of menstrual cycles. Breast tissue is exposed to more estrogen for longer periods of time in women who become pregnant for the first time after age 35 or who never become pregnant.
Taking hormone therapy for symptoms of menopause
Hormones, such as estrogen and progesterone, can be made into a pill form in a laboratory. Estrogen, progestin, or both may be given to replace the estrogen no longer made by the ovaries in postmenopausal women or women who have had their ovaries removed. This is called menopausal hormone therapy (MHT) or hormone replacement therapy (HRT). Estrogen therapy that began close to the time of menopause is associated with an increased risk of developing breast cancer. Estrogen therapy that began at or after menopause is associated with an increased risk of developing endometrial cancer and total cardiovascular disease, especially stroke. The risk of breast cancer does not decrease after women stop taking estrogen.
Combination hormone therapy (HT) is estrogen combined with progestin. This type of HT increases the risk of breast cancer. Studies show that when women stop taking estrogen combined with progestin, the risk of breast cancer decreases.
Radiation therapy to the breast or chest
Radiation therapy to the chest for the treatment of cancer increases the risk of breast cancer, starting 10 years after treatment. The risk of breast cancer depends on the dose of radiation and the age at which it was given. The risk is highest if radiation treatment was used during puberty, when breasts are forming.
Radiation therapy to treat cancer in one breast does not appear to increase the risk of cancer in the other breast.
For women who have inherited changes in the BRCA1 or BRCA2 gene, exposure to radiation, such as that from chest x-rays, may further increase the risk of breast cancer, especially in women who had x-rays before age 20.
Obesity
Obesity increases the risk of breast cancer, especially in postmenopausal women who have not used HT.
Drinking alcohol
Drinking alcohol increases the risk of breast cancer. The level of risk rises as the amount of alcohol consumed rises.
The following are protective factors for breast cancer:
Reproductive history resulting in less exposure to estrogen
A woman's reproductive history can affect the length of time her breast tissue is exposed to estrogen. Early onset of menstruation, late onset of menopause, later age at first pregnancy, and never having given birth have been linked to an increase in estrogen exposure and breast cancer risk. The following reproductive factors decrease the length of time a woman's breast tissue is exposed to estrogen and may help prevent breast cancer:
- Early pregnancy: Estrogen levels are lower during pregnancy. In one study, women who had a full-term pregnancy before age 20 had a lower risk of breast cancer than women who did not have children or who gave birth to their first child after age 35.
- Breast-feeding: Estrogen levels may remain lower while a woman is breast-feeding. Women who breastfed have a lower risk of breast cancer than women who have had children but did not breastfeed.
Taking selective estrogen receptor modulators or aromatase inhibitors and inactivators
Selective estrogen receptor modulators
Tamoxifen and raloxifene belong to the family of drugs called selective estrogen receptor modulators (SERMs). SERMs act like estrogen on some tissues in the body, but block the effect of estrogen on other tissues.
Treatment with tamoxifen lowers the risk of estrogen receptor-positive (ER-positive) breast cancer and DCIS in premenopausal and postmenopausal women at high risk. Tamoxifen is also used to treat metastatic breast cancer and to prevent cancer from recurring after surgery to remove breast tumors. Treatment with raloxifene also lowers the risk of breast cancer in postmenopausal women. With either drug, the reduced risk lasts for several years or longer after treatment is stopped. Lower rates of broken bones have been noted in patients taking raloxifene.
Taking tamoxifen increases the risk of hot flashes, endometrial cancer, stroke, cataracts, and blood clots (especially in the lungs and legs). The risk of having these problems increases markedly in women older than 50 years compared with younger women. Premenopausal women who have a high risk of breast cancer may benefit the most from taking a low dose of tamoxifen, which may decrease breast cancer risk while also reducing some side effects of the drug. The risk of endometrial cancer lasts for 5 years after tamoxifen is stopped, but the risk of cataracts or blood clots does not last long. Talk with your doctor about the risks and benefits of taking this drug.
Taking raloxifene increases the risk of blood clots in the lungs and legs but does not appear to increase the risk of endometrial cancer. In postmenopausal women with osteoporosis (decreased bone density), raloxifene lowers the risk of breast cancer for women who have a high or low risk of breast cancer. It is not known if raloxifene would have the same effect in women who do not have osteoporosis. Talk with your doctor about the risks and benefits of taking this drug.
Other SERMs are being studied in clinical trials.
Aromatase inhibitors and inactivators
Aromatase inhibitors (anastrozole, letrozole) and inactivators (exemestane) lower the risk of recurrence and of new breast cancers in women who have a history of breast cancer. Aromatase inhibitors also decrease the risk of breast cancer in women with the following conditions:
- Postmenopausal women with a personal history of breast cancer.
- Women with no personal history of breast cancer who are 60 years and older, have a history of DCIS with mastectomy, or have a high risk of breast cancer based on the Gail model tool (a tool used to estimate the risk of breast cancer).
In women with an increased risk of breast cancer, taking aromatase inhibitors decreases the amount of estrogen made by the body. Before menopause, estrogen is made by the ovaries and other tissues in a woman's body, including the brain, fat tissue, and skin. After menopause, the ovaries stop making estrogen, but the other tissues do not. Aromatase inhibitors block the action of an enzyme called aromatase, which is used to make all of the body's estrogen. Aromatase inactivators stop the enzyme from working.
Possible harms from taking aromatase inhibitors include muscle and joint pain, osteoporosis, hot flashes, and feeling very tired.
Risk-reducing or prophylactic mastectomy
Some women who have a high risk of breast cancer may choose to have a risk-reducing or prophylactic mastectomy (the removal of one or both breasts when there are no signs of cancer). After surgery, the risk of breast cancer becomes much lower in these women, and most feel less anxious about their risk of breast cancer. Some women diagnosed with breast cancer may decide to have a healthy breast removed at the same time the breast with cancer is removed. This is called contralateral prophylactic mastectomy. However, it is very important to have a cancer risk assessment and counseling about the different ways to prevent breast cancer before making any decision about surgery.
Ovarian ablation
The ovaries make most of the estrogen that is made by the body. Treatments that stop or lower the amount of estrogen made by the ovaries include surgery to remove the ovaries, radiation therapy, or taking certain drugs. This is called ovarian ablation.
Premenopausal women who have a high risk of breast cancer due to certain changes in the BRCA1 or BRCA2 gene may choose to have a risk-reducing oophorectomy (the removal of both ovaries when there are no signs of cancer). This decreases the amount of estrogen made by the body and lowers the risk of breast cancer. Risk-reducing oophorectomy also lowers the risk of breast cancer in average-risk premenopausal women and in women with an increased risk of breast cancer due to radiation to the chest. However, it is very important to have a cancer risk assessment and counseling before making this decision. The sudden drop in estrogen levels may cause the symptoms of menopause to begin. These include hot flashes, trouble sleeping, anxiety, and depression. Long-term effects include decreased sex drive, vaginal dryness, and decreased bone density.
Getting enough exercise
Women who take part in physical exercise have a lower risk of breast cancer.
It is not clear whether the following affect the risk of breast cancer:
Hormonal contraceptives
Hormonal contraceptives contain estrogen or estrogen and progestin. Some studies have shown that women who are current or recent users of hormonal contraceptives may have a slight increase in breast cancer risk. Other studies have not shown an increased risk of breast cancer in women using hormonal contraceptives.
In one study, the risk of breast cancer slightly increased the longer a woman used hormonal contraceptives. Another study showed that the slight increase in breast cancer risk decreased over time when women stopped using hormonal contraceptives.
More studies are needed to know whether hormonal contraceptives affect a woman's risk of breast cancer.
Chemicals in the environment
Scientists are studying whether exposure to chemicals in the environment may increase a woman's risk of breast cancer. Studies of this kind can be difficult to conduct and interpret for many reasons:
- It is hard to determine the specific chemicals people have been exposed to in the past. It can take decades after a potential exposure before cancer develops, and a person may not be aware of or remember the past exposure.
- Even if a chemical is shown in a laboratory test to cause cancer, this does not necessarily mean it will cause cancer in people exposed to that chemical in the environment. A chemical may cause cancer when tested at high levels in laboratory studies but not at the lower levels seen in the environment.
- Individual chemicals are likely to cause only a small increase in risk, and it can be difficult to detect that increase in the context of the other factors that may influence a woman's risk of breast cancer.
These reasons make it hard to know which chemicals, if any, may increase the risk of breast cancer. More studies are needed to know whether chemicals in the environment affect a woman's risk of breast cancer. To learn more, visit Environmental Carcinogens and Cancer Risk.
Studies have shown that some factors have little or no effect on the risk of breast cancer.
The following have little or no effect on the risk of breast cancer:
- Having an abortion.
- Making diet changes such as eating less fat or more fruits and vegetables.
- Taking vitamins, including fenretinide (a type of vitamin A).
- Cigarette smoking, both active and passive (inhaling secondhand smoke).
- Using underarm deodorant or antiperspirant.
- Taking statins (cholesterol -lowering drugs).
- Taking bisphosphonates (drugs used to treat osteoporosis and hypercalcemia) by mouth or by intravenous infusion.
- Changes in your circadian rhythm (physical, mental, and behavioral changes that are mainly affected by darkness and light in 24 hour cycles), which may be affected by working night shifts or the amount of light in your bedroom at night.
Cancer prevention clinical trials are used to study ways to prevent cancer.
Cancer prevention clinical trials are used to study ways to lower the risk of developing certain types of cancer. Some cancer prevention trials include healthy people who may or may not have an increased risk of cancer. Other prevention trials include people who have had cancer and are trying to prevent recurrence or a second cancer.
The purpose of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include eating fruits and vegetables, exercising, quitting smoking, or taking certain medicines, vitamins, minerals, or food supplements.
New ways to prevent breast cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about breast cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Breast Cancer Prevention. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/breast/patient/breast-prevention-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389410]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2025-02-12
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

